Allergies vs. Non-Allergies
24 November 2024
Recently, on a facebook post where I was whinging about my allergy to coconut and specifically not asking for advice (which, FB being FB, I managed to get a lot of anyway), I got a comment that contained the following text.
… “allergy” is a highly specific type of immune reaction that releases histamine. Most people who claim to be “allergic” to everything under the sun have either aversions, sensitivities or at worst intolerances. Nothing wrong with that (sensitivities can cause discomfort and irritation), but only a true allergy can send you to the ER or worse.
I’m bringing this up because I used to be That Guy™ and I’m trying to be better about these things. I have learned more since those days.
Note, that while I understand more about the immune system than here, I’m deliberately simplifying for a non-immunology audience, and will, no doubt, lead so some level of inaccuracy. As the joke goes, “The thing is, the immune system is very complicated …”.
The Classic Allergy
The classic allergy is triggered by an Immunoglobulin E response. Immunoglobulin E is part of the adaptive immune system when it’s presented with an antigen (typically, a protein) that it recognizes (or has been told it should learn to recognize).
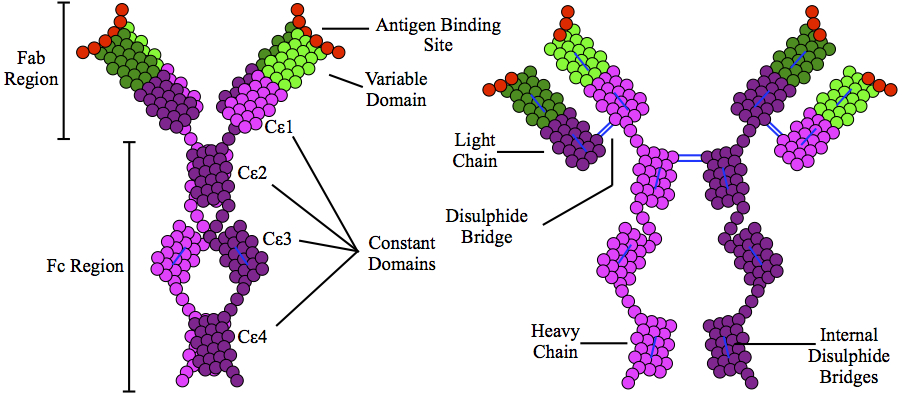
So then what happens? You’ve got a lot of these little antibodies floating around. IgE proteins circulating in the blood don’t release histamine on their own, they are messengers.
IgE primes the IgE-mediated allergic response by binding to Fc receptors found on the surface of mast cells and basophils. (source)
…And according to this paper, also B cells.
So, basically, it collides into an immune system cell that is looking for an antibody to respond to.
I’m going to focus on mast cells here, because they’re the primary releaser of histamine, and often responsible for the histamine reaction that anti-histamines are taken to stop.
Shampoo, My Bane
Let’s travel back in time to February 7, 1977, a day I got a new shampoo sample in the mail. I needed to wash my hair before my dad and I went out to the opening night of Ralph Bakshi’s Wizards, so I used the new shampoo. I sneezed through the entire movie.
Prior to that date, I’d washed my hair without consequence and had used the same shampoo for years.
After that one sample trial, I was also allergic to my regular shampoo and would go into sneezing fits.
For years after that, I’d just take an antihistamine two hours prior to washing my hair, and I’d look for “new and improved” formulas for shampoos I’d previously been allergic to.
By the mid-nineties, I was rotating 6-8 bottles of shampoo to try to mitigate allergy onset. I wasn’t always allergic the first time I used one, but I’d definitely be allergic by the time I finished the bottle. My husband (who’d had a previous life as a bench chemist in soap research) narrowed it down to the sulfates, which were pretty impossible to avoid at that time.
It wasn’t until about ten years ago that we pieced together that it was coconut derivatives I was allergic to. This also extended to other products: I had to avoid eating coconut (not always easy as it’s a vegan substitute for lard), and I also had mouth problems that led to needing to use sulfate-free toothpastes. This also explained why I felt unwell after eating certain foods, e.g., Thai food, that used coconut.
A Scary Non-Allergy
Back when I was diagnosed with fibromyalgia, I was put on gabapentin. That can cause edema (swelling) in the lower limbs, but I had a specific reaction all through my body, but worst in my legs and arms: I would leak clear fluid when I got acupuncture. My acupuncturist had never seen that response before. I’d wound up in the ER as a result when it got really concerning and I had skin blistering (not the first time, but it was really bad this time), so the doc added a classic allergy panel to my blood tests. No IgE elevation was found, but we pulled me off that med.
Years later, my mom was out of her main pain meds, but was on a low dose of gabapentin, and so I added a second one, and she also managed to to to the ER for randomly leaking fluid out of her skin.
Since everyone’s adaptive immune system learns based on their exposures, and my mom and I have had significantly different diets, plus lived in significantly different areas over our lives, it’s far more likely that this happened to be an innate immune system response (with some genetic aspect) rather than an adaptive one.
Mast Cells
Which is where we get to mast cells, the switchboard of the innate immune system.
The most interesting of the books I’ve read about mast cells is Lawrence B. Afrin’s Never Bet Against Occam. He talks about various cases of mast cell disorders that have really peculiar side effects, including “severe magnesium deficits cured by antihistamines.”
In a normal world, you’d never expect taking antihistamines to cure magnesium deficiencies, right? Clearly some process the mast cells triggered were over-using magnesium for some reason, making the person chronically deficient.
Mast cells are implicated in the genesis of both Type I and Type II Diabetes. (Check out the cool photo in that paper of the bags of histamines, shown as black circles, in the cytoplasm.) There’s also evidence that mast cells are involved in the development of congestive heart failure.
Basically, mast cells can wreak havoc all over the place, with or without the direct involvement of Immunoglobulin E, and many of those things will kill you (eventually more often than immediately, granted).
And Then There’s the Patch
I have a medical patch I wear for a week at a time. I take an antihistamine, but one week the skin was broken and I had a couple of small scabs, so I moved to two antihistamines a day. This photo was taken after that change. Next to the obvious angry welt, you can see the shadow of one that’s two weeks old.

So, is that a true allergy? It itches and feels like it’s a histamine reaction. It calms down with applied steroids after patch removal, so that’s how we’re managing it.
In this case, it’s a reaction not to the outer adhesive, which extends beyond the margins of angry red, but instead the actual product delivery matrix. Since that’s the same (for this med) regardless of brand, changing brands wouldn’t help.
This paper talks about the differences between irritant contact dermatitis (ICD) and allergic contact dermatitis (ACD). If it calms down within 48 hours (which mine does not), it may be ICD. ACD takes far longer to resolve.
Famously, the most common classic contact medical contact dermatitis is latex. But there’s a long history of other forms of medical allergies including to adhesives. Further, there are other forms of allergic dermatitis including nickel allergy (which I also have).
Note that for nickel, there’s no protein involved in the metal, so it can’t be a classic allergy. But it’s still called allergic contact dermatitis. It’s not a minor thing, either, as there are significant systemic risks to exposure.
This is a long-winded way to answer: it doesn’t matter if my patch reaction is a classic allergy or not if it doesn’t affect the treatment plan. (And it does not.)
Hope that those of you who, like me, felt that things that weren’t IgE reactions weren’t really allergies understand that things are rather more complicated. Ultimately, mast cells can still cause the same level of havoc with or without the Immunoglobulin E setting off the cascade.
Photo by Simon Kadula on Unsplash
Immunoglobulin E drawing courtesy of Sabban, Sari (2011) Development of an in vitro model system for studying the interaction of Equus caballus IgE with its high-affinity FcεRI receptor (PhD thesis), The University of Sheffield (CC BY-SA 3.0)